The voice we have, and how we make a voice, is typically not anything we pay much attention to, unless it begins to fail us. Understanding how a voice is made as well as how to take care of your voice is key in ensuring the best possible quality and reliability of your voice.
Phonation: Not Just the Vocal Cords
Phonation refers to the process by which we make a voice. While most people believe a voice is produced by the vocal cords, the vocal cords are actually only part of the process. Producing a voice is actually a highly coordinated action that also involves the lungs, the muscles of respiration (breathing) as well as the muscles of the larynx (voice box). When we make a voice, all of these work together to produce the sound we hear.
The quality of the voice produced, therefore, is dependent on several different variables. If one of these components is not working properly, the voice produced may not sound “normal.” When you notice a change in your vocal quality, this is a signal there has been a change somewhere in the system.
How a Voice is Produced
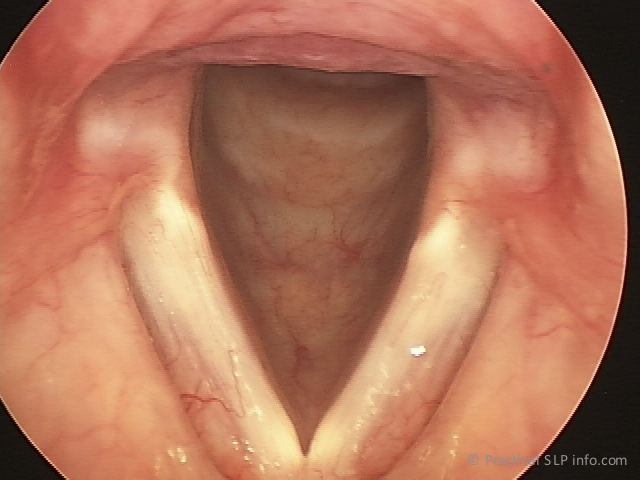
The vocal cords, of course are very important in producing a voice. They are positioned at the top of the trachea, or windpipe, and have the ability to open and close. See images of abducted and adducted glottis.
When we breathe, the vocal cords are open, but they come together in order to make a voice or phonate. The vocal cords coming together, however, will not result in a voice. In fact, the vocal cords do not vibrate independently. In order to produce a voice, the vocal cords must come together, while simultaneously, air from the lungs is exhaled through them in a sufficient manner. The flow of air through the closed vocal cords causes vibrations…the sound we hear as a voice!
Consider how leaves rustle in the wind. Vocal cords vibrate like leaves in the wind. Without airflow or “wind,” the vocal cords are still, and no sound will be produced. In this sense, you can understand then, how we exhale the air is just as important as the vocal cords in terms of producing a voice.
Dysphonia: When Hoarseness
Should Be Addressed
Dysphonia is a general term referring to an abnormal voice. Dysphonia usually happens to everyone at some point, and typically resolves without intervention. One common example of this is a laryngitis that may occur with a virus. As the virus resolves, the voice usually returns to normal on its own.
There are times, however, when dysphonia does not improve. In those cases, it is good to see your doctor. In general, a dysphonia may not be an indication of a serious health issue, but it may not improve, or may even become worse, without proper diagnosis and care.
Although changes in the voice are common and rarely worrisome, there are indications when voice changes should prompt you to see your doctor:
- Dysphonia that Lasts More than 2-3 Weeks Without any Sign of Improvement
- Dysphonia that Begins without a Reason (No Illness, etc.)
- Voice Changes that Get Worse Over Time
- Loss of Pitch Range
- Loss of Volume
- Loss of Voice Control
- Sudden Voice Changes
As a practice with a large oncology patient population, we always encourage any patient with a history of head and neck cancer to contact us immediately if they notice any of the following voice symptoms:
- Pain when Voicing
- Changes in your Voice
- Dysphonia and Simultaneous Ear Pain
- Dysphonia and Difficulty Breathing
- Dysphonia and Interference with Breathing
- Dysphonia and Coughing Up Blood (Even Small Amounts)
Although there may be nothing worrisome present, it is always best to have your doctor evaluate your symptoms.