The type of voice disorder you have will largely determine the appropriate treatment and for this reason, it is extremely important to understand the reason(s) for the voice disorder. In some cases, there may be various options for treatment and your doctor and/or SLP will educate you thoroughly in this regard.
There are two main types of voice disorders, although it is not uncommon to have a combination of the two. In some cases, an organic disorder can result in the development of a functional disorder. For this reason, the best management of your voice disorder may be a combination of treatments.
There are two main types of voice disorders, although it is not uncommon to have a combination of the two. In some cases, an organic disorder can result in the development of a functional disorder. For this reason, the best management of your voice disorder may be a combination of treatments.
Organic Disorders
An organic disorder refers to a problem with the mechanisms of phonation and are classified into two categories:
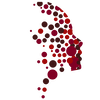
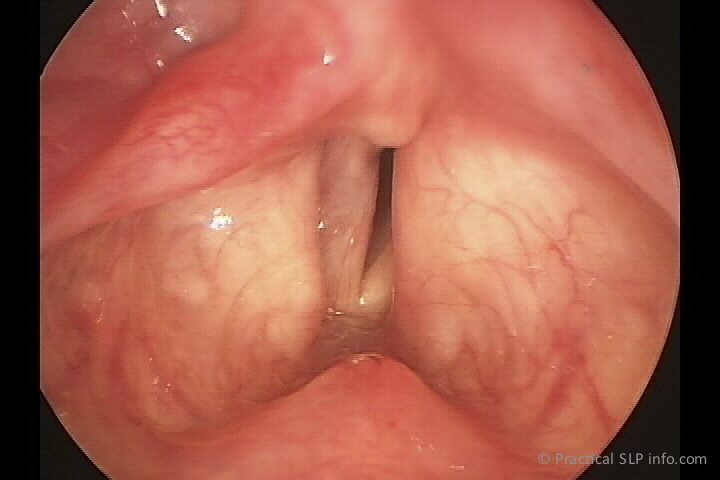
- Structural: A structural disorder refers to a problem with the voice mechanism itself. In this case, there may be fluid in the vocal cords, polyps/cysts interfering with closure and vibration, etc.
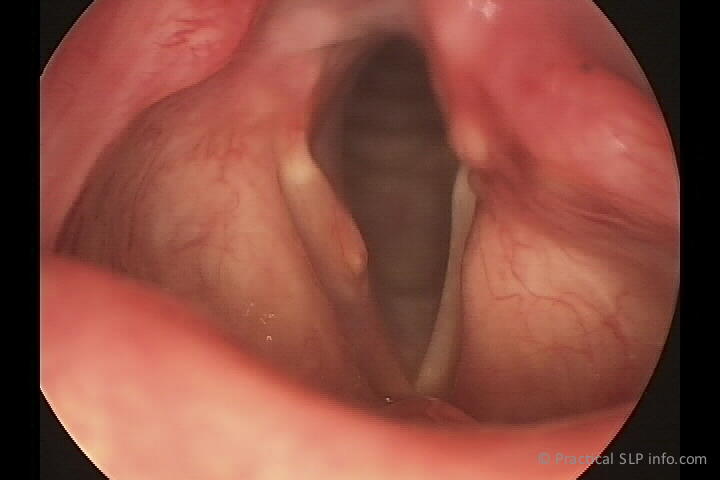
- Neurogenic: A neurogenic voice disorder refers to a disruption in the nerves controlling the larynx. Common examples of this include complete or partial vocal cord paralysis. There can also be spasms in the laryngeal musculature that interfere with the ability to produce a voice.
Functional Disorders
A functional voice disorder refers to a problem with the manner in which a voice is produced and can be affected on many different levels. Voicing, or how we produce a voice, does not require conscious thought or effort. This is because a signal is sent from the brain that automatically results in the coordinated pattern/event we call voicing. For various reasons, however, this pattern can become altered, resulting in behaviors that are interfering with the production of a clear voice.
In some cases, a functional disorder may arise as a result of an organic disorder. For example, if a vocal cord cyst is interfering with the closure of the vocal cords, there may (unconsciously) be more force or effort to close the vocal cords in light of the obstruction. This extra muscle effort can result in a functional disorder, especially if it is continued over an extended period of time.
Functional voice disorders may also have an inconsistency to them, becoming better or worse at different times. It is even possible to have a very normal voice at times, while at other, a significant dysphonia may be present.
Although there may be a degree of variability noted in organic voice disorders, this dysphonia tends to be more consistent.