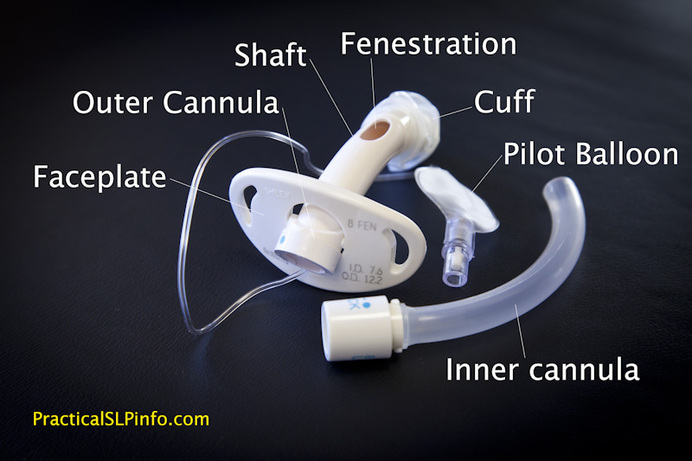
Although several varieties of tracheostomy tubes exist, the general anatomy remains the same. Some specialty or custom tubes may have different/alternate features, the general “anatomy” of the tube is essentially the same.
Faceplate
This is the “collar” of the trach tube, to which the ties or sutures are connected to secure the tube in place. On this you will see numbers and letters that tell your healthcare provider what kind of trach tube you have in place as well as the dimensions of the tube.
OUter Cannula
Most tubes have an “outer” and an “inner” tube or cannula. The outer cannula is connected to the face plate and stays in place until it is time for your tube to be replaced. The width, or diameter, of the outer cannula takes up space in your trachea. If the outer cannula diameter (O.D.) is too large in comparison with your trachea, there may be difficulty using certain speaking valves.
Shaft
This refers to the portion of the tube behind the face plate. In other words, the part of the tube that is inside the body. Standard adult tracheostomy tubes are typically ~75mm in length which is generally sufficient for most adults. For necks that may be thicker in diameter, longer tracheostomy tube are available. This means the shaft will be longer than the standard, however, the portion of the tube in front of the face plate is usually the same length as a standard tube.
Curvature
The curvature of the tube refers to the area where there is a bend in the shaft. The curvature is generally standardized across tubes although custom tubes may be ordered to accommodate a different location and/or angle of curvature. There are some tubes that are flexible as well, allowing the tube to curve according to the patient’s anatomy.
The curvature is an important feature of the tracheostomy tube. In order to be effective, the tube must be rigid enough to maintain an open airway. It’s also important that the shaft of the tube not come in contact with the trachea once it passes through the tracheotomy site. The tissues of the trachea are somewhat delicate and direct contact with the trach tube may result in injury/trauma to the trachea.
|
The curvature is specified so that the shaft of the tube passes essentially horizontally through the soft tissues of the neck, enters the trachea, and the curvature should ensure the shaft of the tube is “floating” within the trachea. Like a tube within a tube. If the curvature is not appropriate for the patient, the tube may then rest or even push against the trachea, likely causing damage.
|
Fenestration
A fenestration is a hole in the shaft of the tracheostomy tube, above the curvature, and therefore also above the cuff of a cuffed trach tube. The purpose of a fenestration is to allow for airflow upward and through the vocal cords. Without airflow through the vocal cords, a tracheostomy patient will not be able to produce a voice. For more information regarding voice production, see How a Voice is Produced.
A fenestration is not necessary to be able to talk with a tracheostomy tube, although it will likely improve the loudness and ease of producing a voice. For more information, see Speaking with a Tracheostomy Tube.
On a fenestrated tube, there is a fenestration in the outer cannula. In order for the fenestration to be of any benefit for voicing, however, the inner cannula must also be fenestrated.
There are advantages and disadvantages to fenestrated tubes. More information on this topic can be found in Fenestrated vs. Non-Fenestrated Tubes.
Cuff
The cuff of a tracheostomy tube is a balloon-like structure attached to the outer cannula below the level of the curvature. A cuff can be inflated with air to fill the space in the trachea between the tracheal wall and the outer cannula. When a cuff is not needed, however, it can be deflated as well. There are various types of coughs as well as reasons for using cuffed tracheostomy tubes. For more information on the use of cuffed trach tubes, see Cuffed vs. Cuffless Tubes.
Pilot Balloon
This is a small plastic balloon with a valve seal that is attached to the shaft of the balloon by a lead line. The pilot balloon lead line is usually attached to the outer cannula near the face plate. The cuff is inflated and deflated via this balloon and the status of the cuff inflation can also be determined fairly well by the inflation status of the pilot balloon. Since the cuff itself sits deep within the trachea, it is impossible to see the cuff status directly. However, if the pilot balloon is inflated, this is an indication the cuff is inflated as well. Similarly, if the balloon is flat, or deflated, this is an indication the cuff is likely deflated.
Although the pilot balloon is an indication regarding the status of the cuff, it is impossible to determine the exact degree of inflation vs deflation based on the pilot balloon alone. For more information regarding cuff status, see Proper Cuff Inflation.
Inner Cannula
The inner cannula sits inside the outer cannula and is designed to be removed and cleaned or removed and replaced. As mucous builds up within the inner cannula (normal) the airway is narrowed. By removing the inner cannula, the airway is improved as the patient is able to breath freely through the space of the outer cannula. This is especially important in the event of a mucous plug that may block the entire inner cannula. The resulting inability to breath is quickly corrected by removing the inner cannula.