I woke up from surgery with a tracheostomy. Why?
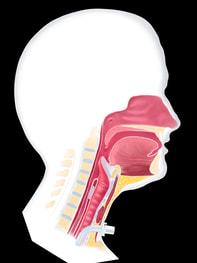
Although this may have been presented as “a possibility” on the surgical consent forms you signed, your doctor determined a need for placing a tracheostomy tube. This is usually based on possible post-operative swelling and inflammation of the structures in the upper airway (the throat and mouth), which may make it difficult to breath. Avoiding an emergency tracheotomy is always good as this also avoids the potential for hypoxia, or alack of oxygen to the brain which can lead to neurologic damage.
When can my tracheostomy be removed?
Although many patients are anxious to be decannulated, or have their tracheostomy tube removed, only your doctor can determine when this is appropriate. In some cases, you will be monitored over time using a tracheostomy tube cap to help determine how well you can breathe through your nose and mouth. It is important to remember that your doctor will always strive to remove the tracheostomy as soon as is safely possible. If it is not considered to be a safe proposition, however, the need for a continued tracheostomy will be explained to you.
Why did my doctor tell me to use a humidifier?
Breathing through a tracheostomy tube means you are not inhaling through your nose/mouth. Normally, the air that is inhaled through the nose/mouth is warmed and humidified as it passes through those structures. Air entering the lungs directly through a tracheostomy tube does not receive the same benefit. Humidified air helps the lungs function properly and also helps to keep secretions thinner, and easier to clear. Non-humidified air can dry out the lungs as well as the mucous, making it more difficult to cough and clear mucous and also increasing the risk for mucous plugging.
If I am not able to speak, why to I need to wear a speaking valve?
In some cases, surgical changes can make it difficult to speak and be understood. Even if you are not able to speak, a speaking valve can offer other benefits. For example, it may allow for a more productive (stronger cough). In some cases, it can help with swallowing. By restoring airflow through the vocal cords and throat, a speaking valve can also help the throat to function more normally. Your SLP can answer any specific questions you may have in this regard.
How often do I need to clean my tracheostomy tube?
It is always important to follow the guidelines set by the manufacturer of the tube and your nurse can typically assist you with this. At a minimum, a tracheostomy tube should be cleaned once daily, although it may be necessary to clean/replace your inner cannula more frequently. Your doctor or SLP can assist you with specific questions in this regard.
I was told to use saline bullets. Why?
Saline bullets are used to provide quick, temporary moisture to the pulmonary air passages and lungs and are most commonly used to correct issues related to inadequate humidification for patients with artificial airways (tracheostomy. Normally, the air that is inhaled through the nose/mouth is warmed and humidified as it passes through those structures. Air entering the lungs directly through a tracheostomy tube does not receive the same benefit.
Without proper humidification, the lungs may become somewhat dry and not function as they should. Also, lung secretions can become thick and dry, difficult to cough and may even result in mucous plugging.
Saline bullets help restore moisture to dry lung tissues, helping both with adequate lung function as well as making secretions easier to manage. Click here to see how to use saline bullets.
Why do I need to have my tracheostomy tube changed when I change my inner cannula as directed?
In many cases, your doctor may decide to change the entire tracheostomy tube. Typically this is done to reduce the risk of bacterial colonization on the tube which may lead to infection. In other cases, if you’ve had an infection of the lungs or trachea, your doctor may choose to change your tracheostomy tube to ensure no further contamination by the infection.
If you have a cuffed tube and the cuff is no longer functional, the tube must be replaced, as there is no way to repair a damaged cuff.
How often do I need to suction myself?
The use of suction depends on how much mucous you have to clear. Having a tracheostomy tube, without a speaking valve, means that coughing is different. It is much more difficult to produce a strong and effective cough with a tracheostomy and you may need suction to help clear the mucous from your airway. As a general rule, the thicker the mucous, the more difficult it will be to cough and clear this. Suction can be very helpful in removing mucous and secretions from the airway.
What happens if my tracheostomy tube comes out accidentally?
It is important to always try to replace the tube immediately if possible. The opening for the tracheostomy tube will close spontaneously without a tube in place. The longer the tube is out, the potential increases for the opening to become too small or even close entirely, preventing tube replacement.
Be sure the tube is clean before replacing into the neck!
My doctor told me only loose ties around my neck to hold the trach tube. Why?
Surgical wounds always need adequate blood supply in order to properly heal. If you have wounds and/or reconstructive grafts in the neck region, trach ties that are too tight can cut off blood flow to the area and prevent proper healing. If you are told to use only loose trach ties, it is very important to ensure there is no pressure on the neck tissues from the ties.
Why is my swallowing more difficult following a tracheotomy?
Many patients reports changes in their swallowing following a tracheostomy. Although many patients swallow very well following a tracheostomy, there are several reasons why a change in swallowing may be noticed.
For this reason, should you notice any changes in your swallow ability, or begin coughing, choking during eating, it is extremely important to notify your doctor/SLP. Following an evaluation, the SLP staff be able to better manage your swallowing for the best function possible.
If at any time you notice food/drink material being coughed and expelled from the tracheostomy tube, you should always contact your doctor and/or SLP immediately. This may be an indication of a swallowing problem that could have very severe health implications.
Subglottic Pressurization
The closing of the vocal cords also plays a very important role in the swallow process. By closing during the swallow, the vocal cords prevent any air from leaving the lungs during the swallow. This subglottic pressure is important for driving a strong swallow. For more information on how we swallow, see Normal Swallowing (link)
In a tracheostomy patient, even if the vocal cords adduct (close) as they should during the swallow, the typical subglottic pressurization is not achieved since the open tracheostomy tube is creating an opening for air to leave the lungs. As such, many patients may experience swallowing difficulty following their tracheostomy.
A Passy-Muir Speaking Valve (PMV) can be utilized to assist with swallowing difficulties when subglottic pressurization appears to be a contributing factor. For this reason, if you have been provided with a PMV, it is always recommended you are wearing the valve during meals, but also as often as possible, while awake, is ideal in this regard, as it will also help with the regular swallowing of saliva and other secretions throughout the day.
Hyolaryngeal Movement
During a normal swallow, the larynx (voice box), along with other attached muscles/structures, moves upward and outward. This is referred to as hyolaryngeal movement and can be observed when you watch or feel your Adam’s apple (thyroid cartilage) move up and down during a swallow.
In normal human anatomy, the larynx is attached to the trachea, through which the tracheostomy tube has been inserted and rests following a tracheostomy. In some cases, the tube can contribute to less hyolaryngeal movement as a result. Any changes in swallowing following a tracheostomy should always be reported to your doctor and/or SLP staff. Although the tracheostomy may not be contributing to any perceived swallowing problem, proper evaluation of the swallow function should be conducted to ensure the patient is eating as safely and effectively as possible.
Why is it harder to breath with a speaking valve?
Inhaling through a speaking valve adds a small degree of resistance to the inhalatory airflow. Although most patients can tolerate this well, there are a small percentage that cannot.
Typically speaking, however, if patients notice difficulty tolerating a speaking valve, it is associated with increased exhalatory difficulty. To use a speaking valve, particularly a Passy-Muir Speaking Valve, the exhaled air is required to travel upward through the nose and mouth. If the flow of air is restricted in any way through this region (i.e., swelling, etc), then there will be more effort required to exhale through these structures. For this reason, many patients are unable to tolerate this form of speaking valve.
I thought a speaking valve was for talking. Why do I have to wear it for eating too?
Subglottic pressurization
The closing of the vocal cords plays a very important role in the swallow process. By closing during the swallow, the vocal cords prevent any air from leaving the lungs during the swallow. This subglottic pressure is important for driving a strong swallow. For more information on how we swallow, see Normal Swallowing.
In a tracheostomy patient, even if the vocal cords adduct (close) as they should during the swallow, the typical subglottic pressurization is not achieved since the open tracheostomy tube is creating an opening for air to leave the lungs. As such, many patients may experience swallowing difficulty following their tracheostomy.
A Passy-Muir Speaking Valve (PMV) can be utilized to assist with swallowing difficulties when subglottic pressurization appears to be a contributing factor. For this reason, if you have been provided with a PMV, it is always recommended you are wearing the valve during meals, but also as often as possible, while awake, is ideal in this regard, as it will also help with the regular swallowing of saliva and other secretions throughout the day.
In a tracheostomy patient, even if the vocal cords adduct (close) as they should during the swallow, the typical subglottic pressurization is not achieved since the open tracheostomy tube is creating an opening for air to leave the lungs. As such, many patients may experience swallowing difficulty following their tracheostomy.
A Passy-Muir Speaking Valve (PMV) can be utilized to assist with swallowing difficulties when subglottic pressurization appears to be a contributing factor. For this reason, if you have been provided with a PMV, it is always recommended you are wearing the valve during meals, but also as often as possible, while awake, is ideal in this regard, as it will also help with the regular swallowing of saliva and other secretions throughout the day.