Deflate the cuff
For the methods described here, any cuff must be deflated, as much as possible. Even a deflated cuff can take up space in the airway, limiting the airflow available to speech. Because of this, it’s best to deflate the cuff as much as possible.
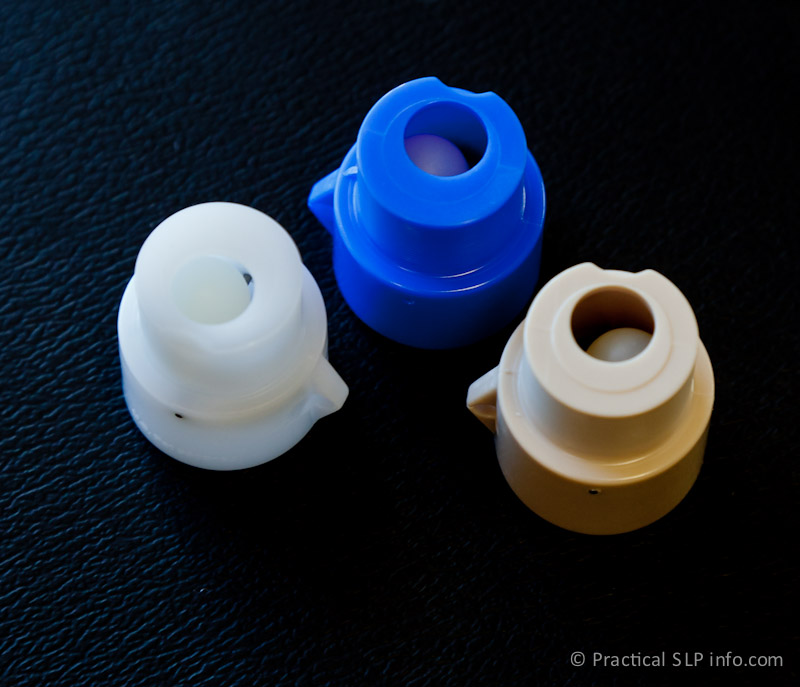
Speaking valves
Speaking valves are the most common method of restoring voice following a tracheostomy. These may also be used in-line with a ventilator in some cases. Although a speaking valve provides excellent voice restoration, these valves are not appropriate for all patients. Your doctor/SLP staff will determine if you are a candidate for a speaking valve and select the most appropriate valve for you. In this practice, there are two main types of speaking valves prescribed and utilized.
Passy-Muir Speaking Valve (PMV)
The PMV is a speaking valve placed as a cap, over the end of the tracheostomy tube. There are various versions, although the technical function is the same across valves.
The PMV is the most commonly used speaking valve in this practice for the many benefits its “positive closure” design offers. Although other speaking valves exist, this is the only one with the “positive closure” feature. The “positive closure” valve means that the valve remains closed until a sufficient amount of inhalation pressure is applied. In contrast, other speaking valves close in response to exhaled air pressure, otherwise they remain open to some degree. There are several benefits to the positive closure design for our patients.
- Speaking: Of course, the primary benefit from this valve is restoring speech to the tracheostomy patient. By remaining closed, the valve redirects exhaled air upward through the vocal cords automatically. No extra time/effort/airflow is required to close the valve.
- Coughing: Because the valve remains in a closed position, except during active inhalation, all cough efforts are directed through the throat and mouth, more similar to normal physiologic function in this regard. This design also helps ensure no air is lost through the tube, leaving the patient able to more effectively cough since there is more air available.
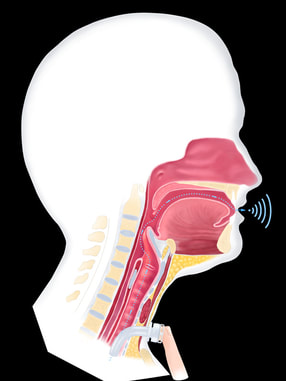
The positive closure feature also means secretions are prevented from entering the tube or the speaking valve which can mean less cleaning and more reliable function as a result. - Swallowing: The closing of the vocal cords also plays a very important role in the swallow process. By closing during the swallow, the vocal cords prevent any air from leaving the lungs during the swallow. This subglottic pressure is important for driving a strong swallow. For more information on how we swallow, see Normal Swallowing.
In a tracheostomy patient, even if the vocal cords close as they should during the swallow, the typical subglottic pressurization is not achieved since the open tracheostomy tube is creating an opening for air to leave the lungs. As such, it is not uncommon to experience swallowing difficulty following a tracheostomy.
The PMV, however because it remains in a closed position during swallowing, allows for subglottic pressure to be maintained, thus helping to restore normal physiology for swallowing. For this reason, in particular, this valve is typically used over other speaking valve options.
It can be difficult, however, for our head & neck patients to safely tolerate a PMV. Because the valve remains closed except during inhalation, the patient must be able to effectively exhale through the passageways of the nose and mouth. For this reason, it may not be appropriate for certain patients. Your doctor/SLP staff can answer any further questions you may have in this regard.
Shikani Speaking Valve
Although the PMV is preferred for its positive closure design, for those patients that are unable to tolerate it, the Shikani Speaking Valve may provide a viable option, especially for the head & neck cancer patients.
This valve is designed with a small plastic ball that forms the valve and the valve itself can be configured different ways to allow for more easy breathing through the tube vs easier valve closure for talking. As a result, this valve design can be better tolerated by those patients who are unable to breath comfortably with the PMV.
ALternatives to speaking Valves
Finger Occlusion
For tracheostomy patients not breathing with the help of a ventilator, the finger occlusion technique is the quickest, easiest and least expensive way to restore speech. For this method, simply use your finger to seal the end of the tube when you want to talk. This will divert the air through the vocal cords (instead of exiting out the tube). After speaking, remove your finger to allow for normal respiration through the tracheostomy.
This technique, however, should only be used when the hands are clean as bacteria can easily be introduced from the fingers to the tube, presenting a potential for infecting the airway and lungs.
This technique, however, should only be used when the hands are clean as bacteria can easily be introduced from the fingers to the tube, presenting a potential for infecting the airway and lungs.
Specialty Tubes
There are certain tracheostomy tubes designed with the sole purpose of allowing for oral speech when more traditional options are not possible. The SLP staff will work with you to ensure your optimal communication/swallowing status and can discuss the potential benefits of these tube options as appropriate. Typically speaking, however, the vast majority of patients can achieve a functional communication status without the need of a specialty tube for this purpose.
Electrolarynx
Although not commonly used, an electrolarynx is an option for producing speech following a tracheostomy. Although speech methods that use the patient’s own voice (produced by the vocal cords) is always preferred, there may be times when this is not possible. For example, in the event the larynx (voicebox) is not functioning properly, or if the patients is unable to have enough airflow through the vocal cords to produce their own voice, then an electrolarynx is an option.