Communicating After Surgery
Usually, one of the greatest concerns a laryngectomee patient and family will have relates to communication. The surgery removes the voice box and therefore will take away your ability to speak as you did before. However, modern advancements in voice restoration have allowed laryngectomees to speak with clear, functional and natural sounding voices, often stronger and clearer than before the laryngectomy surgery. What you are able to use to help you speak will depend on the extent of your surgery as well as your recovery.
Immediately after surgery you will need to use non-verbal ways of communicating. It is important for family members, nurses and doctors to ask “yes/no” questions to communicate with you. You may use a blinking method (once=yes; twice=no), or other such techniques to respond. As you begin to recover more, (after a day or so) the Speech Pathologist in the hospital will come to see you and may give you a communication board or a dry-erase board. If you are unable to write for any reason, a communication board will help greatly. With this board, you can point to various word choices as well as spell out words. Once you feel well enough to write, you can use this as a means to communicate everything you may want.
You will soon realize writing is not nearly as efficient in communicating your thoughts as oral speech. For this reason, one of the earliest goals in your rehabilitative process is for you to be an oral communicator again.
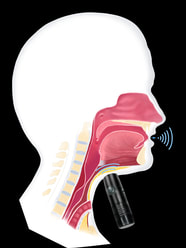
Using an Electrolarynx
An electrolarynx is a device that produces an electronic tone in place of your own voice. This can be used fairly soon after surgery, within a few days, but requires some assistance from a Speech Pathologist to teach you how to use it. Initially this device can be used with a “straw” adapter that is placed in your mouth. Once you begin to heal and the neck is no longer tender, the device is placed on the neck, near the region where your larynx used to be. You will also have to practice a bit so that you can be easily understood. For decades, laryngectomees use this as their primary way of communicating, although with the evolution of the TEP or “tracheoesophageal voice prosthesis, “ the electrolarynx is used much less frequently as a primary means of communication. Many successful TEP users, however, will have this as an alternate means of communication as needed or “just in case.”
The state of Texas provides all laryngectomees with a voucher to be used toward purchasing an electrolarynx. With this voucher, the device can be purchased at no cost to the patient and, as such, is generally advised that patients acquire and learn to use this. Katrina’s office or the hospital can provide you with the voucher application for this purpose.
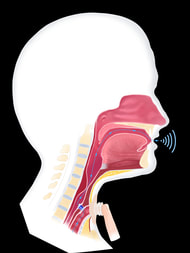
Using a TEP
Most patients, however, will be able to speak using the most advanced methods for voice restoration. This is known as tracheoesophageal voice restoration. With this form of voice restoration, a small hole is made in common wall that is shared by the trachea (windpipe) and the esophagus (food pipe). This procedure is typically conducted during your laryngectomy surgery, although can also be completed later as well. Once you have healed well enough, Katrina will fit a voice prosthesis into the hole or “tract.” This device is referred to as a “tracheoesophageal voice prosthesis” or “TEP.” This device acts as a one-way valve that allows air to pass into the esophagus and flow out of the mouth, but closes when air is not flowing through it to keep food, liquid and saliva out of the trachea.
Listen to A laryngectomy USING A TEP
When using a TEP, voicing is achieved by channeling air from the lungs into the esophagus. Just above the TEP, in the esophagus, and extending into the lower portion of the throat or “pharynx,” there is a segment of tissue that vibrates when air passes through it, similarly to how vocal cords vibrate and make a noise. The “voice” this makes is different from your original voice but it gives you a natural sound source that you can now talk with as you did before the surgery. Katrina will discuss the process of TEP placement and its use with you. You will need therapy to learn how to use and care for the device but this is relatively short-term in nature.
Other Effects of Your Surgery
Because there is no longer any air flowing through the nose after the laryngectomy, you will notice a change in your sense of smell and taste. Your ability to smell will be exactly the same as before the surgery in that the nerves, senses and structures involved in smelling will not be changed in any way. Without the flow of air through the nose, however, the capacity to smell changes. In order to smell scents, odors and aromas around us involves having air pass through the nose, carrying small particles into the nose where they are detected by sensory cells in the nose which are then interpreted by the brain and translated into “smells.” Since no air will be flowing through the nose after your surgery, it will seem as if you can no longer smell things like you could before. Many laryngectomees find it helpful to use their hand to “waft” air into their nose when they attempt to smell. The speech pathology staff will also teach you a technique which will allow you to draw air through the nasal passages and assist with smelling.
Similarly, because our sense of taste is strongly related to our sense of smell, you will notice that foods may no longer taste the way they did before the surgery. The tongue is able to detect five basic tastes: sweet, sour, salt, bitter and savory. Our sense of smell adds to the taste of our food and allows us to recognize the difference between steak and pizza, for example. Once you start eating after surgery, you will notice that your favorite foods may taste quite different from what you remember.
To experience what this is like, a non-laryngectomized person can place a jellybean in their mouth, first holding the nose shut. Chew the jellybean as normal. You will notice the sweetness, but the flavor (orange vs grape for example) is impossible to tell. Then release the nose and inhale. Suddenly, the flavor becomes obvious. This ability to inhale through the nose is lost, and accounts for the notable change in taste following surgery.
The technique the speech pathology staff will teach you is also referred to is the “polite yawn technique". Its works to help move air through your nose, and by doing this, will also improve your ability to taste more accurately. Many laryngectomees have reported this helps foods taste more “normal.” Despite learning this maneuver, you may still not feel as though foods taste as they did before your surgery. Over time, however, generally within the first 6-9 months, most laryngectomees feel as if their foods taste “normal” again.
Swallowing and Eating
Prior to their laryngectomy, many patients often experience difficulty swallowing. It is important to remember that following the laryngectomy surgery, you will no longer have any potential to choke while eating. This is due to the disconnection of the nose, mouth and throat from the airway.
It is important to understand, however, that your swallow will be different. It will feel very different when you first begin to eat following surgery. During the surgery, many of the structures used in swallowing are removed. In removing these, the mechanism or act of swallowing changes. You will notice it “feels” different to swallow. Some patients often report it takes more effort to clear food through the throat. These are common and normal consequences of the surgery. In time, most patients learn to swallow “differently,” but just as effectively as before their laryngectomy.
You will first start eating by being limited to liquids and/or purees and gradually advanced to more solid foods once it is felt you are able to swallow well at each level and have healed sufficiently. This gradual return to eating will also help you become more comfortable with the changes in your swallow.
There are certain cases, however, when difficulty swallowing may need intervention in order for you to return to a normal eating pattern. At any point, should you notice you are not able to swallow certain foods or textures, the speech pathology staff can examine this more thoroughly and develop a plan to improve your swallow function.
Click here to learn more about swallowing as a laryngectomy.
Bathing and Water Activities

Shower Protection
After your laryngectomy, it is very important that you protect your stoma from water getting into it. The open stoma serves as a direct “pipeline” into the lungs. During showers, you can wear a special cover that is designed to keep water away from the stoma. Taking a bath is not generally recommended; however, should you choose to sit in a tub of water, be sure to keep the water level no higher than your navel.
Recreational activities such as swimming, boating, fishing and other water sports are not advised after your surgery as they represent a significant drowning risk. There are, however, centers that specialize in adaptive equipment to allow laryngectomees to participate more safely in these activities. The speech pathology department can assist you with this information should you choose. Without proper adaptive equipment, however, it is strongly advised you avoid such activities following your laryngectomy. With a laryngectomee stoma, should you fall into water, your lungs can fill with water within seconds. You should also always be very cautious when walking near deep water, such as on docks.